Autoimmune
Stem Cell Treatment
Stem Cell Therapy for Hashimoto's: A New Approach to Autoimmune Thyroid Dysfunction
Understanding What's Really Happening in Your Thyroid
Most people with Hashimoto's thyroiditis know the frustration. You take your levothyroxine every morning, your TSH levels look fine on paper, and your doctor tells you everything is under control. But you still feel exhausted. You still struggle with brain fog, weight that won't budge, and a general sense that something isn't right. Stem cell therapy for Hashimoto's offers a different approach, one that addresses the underlying autoimmune process rather than just managing hormone levels. Here's what I've learned after years of working with autoimmune patients: managing hormone levels and addressing the root cause are two very different things.
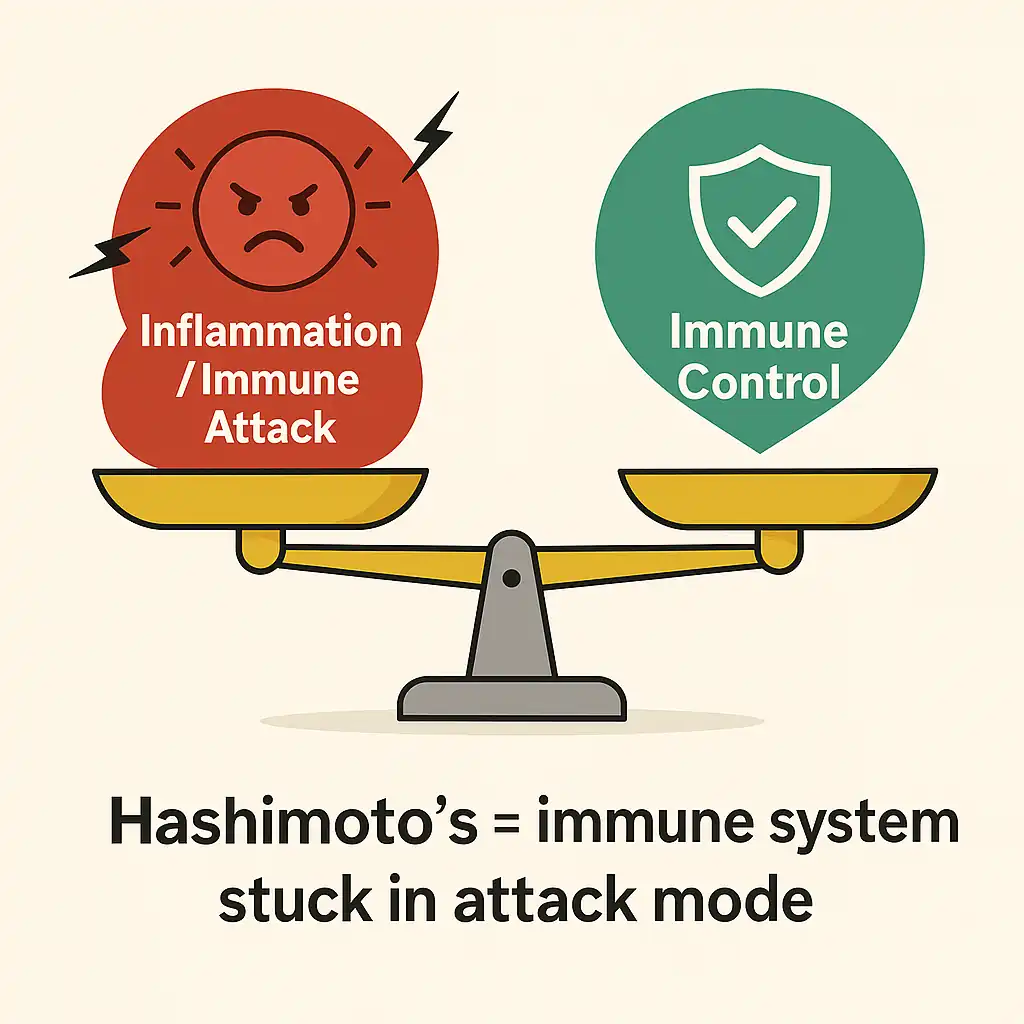
Hashimoto's isn't just a thyroid problem. It's an immune system problem that happens to target your thyroid. The standard approach of replacing thyroid hormones addresses the consequence of the damage, not the cause. Your immune system is still attacking your thyroid tissue, still creating inflammation, still progressing the disease. The levothyroxine just masks that your thyroid is being slowly destroyed.
Stem cell therapy for Hashimoto's takes a fundamentally different approach. Instead of replacing what your damaged thyroid can no longer produce, it works to calm the immune dysfunction that's causing the damage in the first place. The goal isn't to cure Hashimoto's, because autoimmune conditions don't work that way, but to rebalance the immune system, reduce the attack on your thyroid, and potentially slow or halt the progression that makes you feel worse year after year.
What Is Stem Cell Therapy for Hashimoto's Disease?
Stem cells are your body's repair and regulation system. Unlike specialized cells that do one specific job, stem cells remain flexible until your body signals what's needed. They can become different cell types, but more importantly for autoimmune conditions, they can powerfully influence how your immune system behaves.
The mesenchymal stem cells we use have been extensively screened and tested for safety and potency. When delivered intravenously, these cells don't just float around randomly. They respond to inflammatory signals, essentially following the chemical distress calls that inflamed tissue sends out. They migrate toward areas of dysfunction, including your thyroid, and begin releasing anti-inflammatory compounds, immune-regulating factors, and signals that help restore balance.
What makes this particularly relevant for Hashimoto's is that mesenchymal stem cells have a documented ability to influence the specific immune cells involved in autoimmune thyroid destruction. They can help shift the balance away from the inflammatory cells attacking your thyroid and toward the regulatory cells that should be keeping that attack in check.
The Immune Imbalance Driving Your Symptoms
Let me explain what's actually happening in your body, because understanding this helps everything else make sense.
Your immune system has different types of T cells that serve different functions. Th17 cells are pro-inflammatory. They're part of your body's defense system, but in autoimmune conditions, they become overactive and start attacking your own tissue. Regulatory T cells, called Tregs, are supposed to keep the Th17 cells in check. They're the peacekeepers that prevent your immune system from going after things it shouldn't.
In Hashimoto's, this balance is disrupted. You have too many Th17 cells driving inflammation and not enough Tregs suppressing the attack. The result is that your immune system continuously produces antibodies against your thyroid tissue, specifically anti-TPO and anti-thyroglobulin antibodies, while immune cells infiltrate your thyroid gland and cause progressive damage.
This isn't just about your thyroid hormone levels. The chronic inflammation affects your entire system. It contributes to the fatigue that sleep doesn't fix, the brain fog that makes you feel like you're thinking through mud, the weight that accumulates despite eating carefully, and the mood changes that can make you feel like a different person than you used to be. Understanding the connection between stem cells and Hashimoto's means understanding how immune regulation works at the cellular level.
Here's what concerns me about the standard approach: checking your TSH and adjusting your levothyroxine dose does nothing to address this underlying immune dysfunction. Your antibody levels can keep climbing, the inflammation can keep progressing, and your thyroid can keep deteriorating, all while your hormone levels appear "controlled."
The Natural Decline of Your Body's Repair System
There's another factor working against you as you age. Your body's natural supply of mesenchymal stem cells declines significantly over time. By age 35, you've lost approximately 5-10% of your original stem cell count. By age 50, you've lost around 30-50%. By age 70, you've lost about 70-90% of your original capacity.
This matters for autoimmune conditions because mesenchymal stem cells play a crucial role in immune regulation. They're part of how your body naturally maintains the balance between inflammatory and anti-inflammatory responses. When your stem cell numbers drop too low, your immune system loses some of its natural braking mechanism. The overactive inflammatory responses that drive conditions like Hashimoto's become harder for your body to control on its own.
This helps explain why autoimmune conditions often worsen with age, and why some people develop autoimmune diseases later in life that they never had before. The regulatory systems that kept everything in check are gradually declining.
How Stem Cell Therapy Works for Hashimoto's
When stem cells enter your bloodstream, they immediately begin responding to inflammatory signals throughout your body. They're drawn to areas of immune dysfunction, and once there, they start releasing a range of therapeutic factors.
The stem cells produce TGF-beta, which promotes the development of regulatory T cells, the peacekeepers your immune system needs more of. They release prostaglandin E2, which calms overactive immune responses. They secrete hepatocyte growth factor, which supports tissue repair and has antioxidant effects. They produce interleukin-10, a powerful anti-inflammatory signal. And they express IDO, an enzyme that helps create a more tolerant immune environment.
What's particularly interesting is that research has shown these effects directly address the Th17/Treg imbalance that drives Hashimoto's. In animal studies, stem cell treatment reduced the harmful Th17 cells while increasing the protective Treg cells. Thyroid autoantibody levels dropped. Lymphocyte infiltration into the thyroid decreased. And thyroid tissue showed less damage.
The stem cells don't cure the underlying tendency toward autoimmunity. What they do is help reset the immune balance, reduce the inflammatory attack, and give your thyroid a chance to function better without being under constant assault.
The Research Behind This Approach
I want to be transparent about what the research shows, because understanding the evidence helps you make an informed decision.
A 2020 study published in Autoimmunity tested stem cell treatment in a rat model of Hashimoto's thyroiditis. The results were encouraging. Treated animals had significantly lower levels of the antibodies that attack the thyroid compared to untreated controls. There was less visible damage to thyroid tissue and fewer immune cells invading the thyroid gland. Most importantly, the treatment restored balance to the immune system by reducing Th17 cells and increasing regulatory T cells. This is exactly the immune shift we want to see.
Research published the same year in the American Journal of Translational Research looked at combining stem cells with selenium, a mineral that supports thyroid health. The combination worked better than either treatment alone. Thyroid tissue in treated animals returned to near-normal structure. The stem cells also released higher levels of healing factors, including TGF-beta, HGF, and SCF, when selenium was present. This suggests that combining stem cell therapy with targeted nutritional support may enhance the results.
A comprehensive 2022 review in Current Therapeutic Research analyzed over two decades of research on stem cells for Hashimoto's thyroiditis and other autoimmune thyroid disease. The authors concluded that stem cells work primarily by calming the overactive immune response rather than by regenerating damaged tissue. This immune-balancing effect is what makes the therapy particularly promising for autoimmune conditions like Hashimoto's, where the problem isn't tissue damage per se but the ongoing immune attack causing that damage.
Additional research from 2021 confirmed that mesenchymal stem cells can reduce thyroid autoantibody levels specifically by restoring the balance between inflammatory and protective immune cells. The cells achieve this through both the factors they release and through direct cell-to-cell contact with immune cells.
I should be clear: most of this research has been conducted in animal models. Human clinical trials specifically examining Hashimoto stem cell treatment are still limited. But the mechanisms are well-established, the safety profile is excellent, and the consistency of positive outcomes across multiple studies provides a reasonable foundation for considering this approach.
Complete Treatment Experience: What to Expect
The entire procedure takes approximately 60-90 minutes from start to finish. Since we use pre-screened donor cells, there's no need for any extraction procedures from your own body. This makes the treatment straightforward and comfortable.
What Happens During Your Treatment
The treatment involves an intravenous infusion, similar to receiving IV fluids. You'll be seated comfortably, and most patients read, rest, or use their phones during the infusion. There's no sedation required, and you can return home the same day.
The Steps Involved
Here's exactly what happens:
First, we review your thyroid function tests and antibody levels to establish a clear baseline. I want to know your current TPO antibody levels, thyroglobulin antibody levels, TSH, and free T4 before we begin. This gives us concrete markers to track over time.
We prepare mesenchymal stem cells combined with platelet-rich plasma for your infusion. The PRP contains growth factors that support the stem cells' activity and your body's response.
The infusion itself takes 30-45 minutes. The stem cells are delivered directly into your bloodstream, where they begin circulating and responding to inflammatory signals throughout your body.
After the infusion, we monitor you briefly to ensure you're comfortable before you go home.
To enhance results, we complement the stem cell treatment with customized nutritional protocols, including selenium optimization based on that research showing improved outcomes with selenium supplementation. We also provide supplement recommendations, lifestyle modification guidance, and ongoing follow-up monitoring.
Recovery and What to Expect
Your body begins responding to treatment immediately, though the effects develop gradually. Here's the typical timeline:
During the first 48-72 hours, some people experience mild fatigue or low-grade fever as the immune system responds to the stem cells. This actually indicates the treatment is working, that your immune system is engaging with the cells. Rest is encouraged, but normal activities can continue.
Within the first week, most people return to their regular routine within a day or two. Some report feeling more energetic or noticing improved mental clarity early on, though this varies.
Over weeks 2-4, initial improvements often become more noticeable. Better energy levels, improved mood, clearer thinking, or reduced symptoms. These early changes frequently indicate more significant improvements to come.
Months 1-6 is when substantial changes typically occur. The stem cells continue working to rebalance the immune system and reduce thyroid inflammation. Most people experience progressive improvements throughout this period. Thyroid antibody levels may begin to decrease on follow-up testing. Peak benefits often appear between months 3-6.
What's Included in Treatment
Your treatment includes everything involved in the process:
Initial medical consultation and comprehensive thyroid evaluationMesenchymal stem cells plus PRPComplete thyroid panel including antibody levelsThe infusion procedure with medical supervisionAll medical supplies and sterile equipmentPersonalized nutrition program including selenium recommendationsSupplement recommendations based on your specific needsFollow-up monitoring and support
Frequently Asked Questions
Can Stem Cells Help Hashimoto's Disease?
Research suggests that mesenchymal stem cells may help address the underlying immune dysfunction in Hashimoto's disease. Studies have shown that stem cells can reduce thyroid autoantibody levels, decrease inflammatory Th17 cells, and increase protective regulatory T cells in animal models. While human clinical trials are still limited, the documented immunomodulatory effects of stem cells align with what would theoretically benefit Hashimoto's patients. Individual responses vary, and stem cell therapy should be considered as part of a comprehensive treatment approach rather than a standalone solution.
Is Stem Cell Therapy Effective for Hashimoto's Thyroiditis?
The current evidence from animal studies and early research is encouraging. Multiple studies have demonstrated that stem cell treatment can restore thyroid tissue structure, reduce lymphocyte infiltration, and improve immune balance markers in Hashimoto's models. Effectiveness in humans may vary based on disease stage, current antibody levels, and individual factors. Most patients report improvements in energy, mental clarity, and overall wellbeing, though objective measures like antibody levels should be tracked to assess individual response.
Are Stem Cells Used for Autoimmune Thyroid Disease?
Yes, stem cells are being investigated as a treatment approach for autoimmune thyroid diseases including Hashimoto's thyroiditis. Research reviews have documented the ability of mesenchymal stem cells to modulate immune function in various autoimmune conditions. For autoimmune thyroid disease specifically, the therapeutic mechanism involves rebalancing the Th17/Treg ratio and reducing the autoimmune attack on thyroid tissue. This represents a fundamentally different approach than hormone replacement, targeting the immune dysfunction rather than simply managing its consequences.
What Results Can I Expect from Treatment?
The research shows reductions in thyroid autoantibody levels, decreased immune cell infiltration into the thyroid, and restoration of thyroid tissue structure in animal models. In practical terms, many patients report improved energy, better mental clarity, more stable mood, and an overall sense of feeling better. Individual results vary based on disease stage, current antibody levels, and other factors. Progress is typically tracked through follow-up thyroid panels to monitor objective changes alongside symptom improvement.
Conclusion
Stem cell therapy for Hashimoto's disease represents a fundamentally different approach than standard hormone replacement. Instead of managing the consequences of thyroid damage, it addresses the underlying immune dysfunction that drives the condition.
The research demonstrates that mesenchymal stem cells can restore the Th17/Treg balance that's disrupted in Hashimoto's, reduce thyroid autoantibody levels, and decrease the inflammatory attack on thyroid tissue. While most current research has been conducted in animal models, the mechanisms are well-understood, the safety profile is favorable, and the consistency of positive outcomes across multiple studies provides a reasonable basis for considering this approach.
If you're experiencing persistent symptoms despite hormone replacement, or if you're looking for an approach that targets immune dysfunction rather than just its symptoms, stem cell therapy may be worth exploring as part of a comprehensive treatment plan.
The information in this article is for educational purposes only and is not intended as medical advice. Individual results vary. Stem cell therapy for Hashimoto's disease remains an emerging treatment approach with most research conducted in animal models. Statements not evaluated by the FDA or COFEPRIS.
Treatment
- Medical consultation
- 200 to 300 million stem cell IV + 10 billion exosomes+ placenta implant
- Super immune IV + others as need
- Full blood panel
- Recommended supplement to take.
- Recommendation on things to do to enhance wellness.
