Heart, Lung, and other Organs
Stem Cell Treatment
Stem Cell Therapy for Heart Attack Recovery: What You Need to Know
Why Heart Attack Recovery Is So Difficult
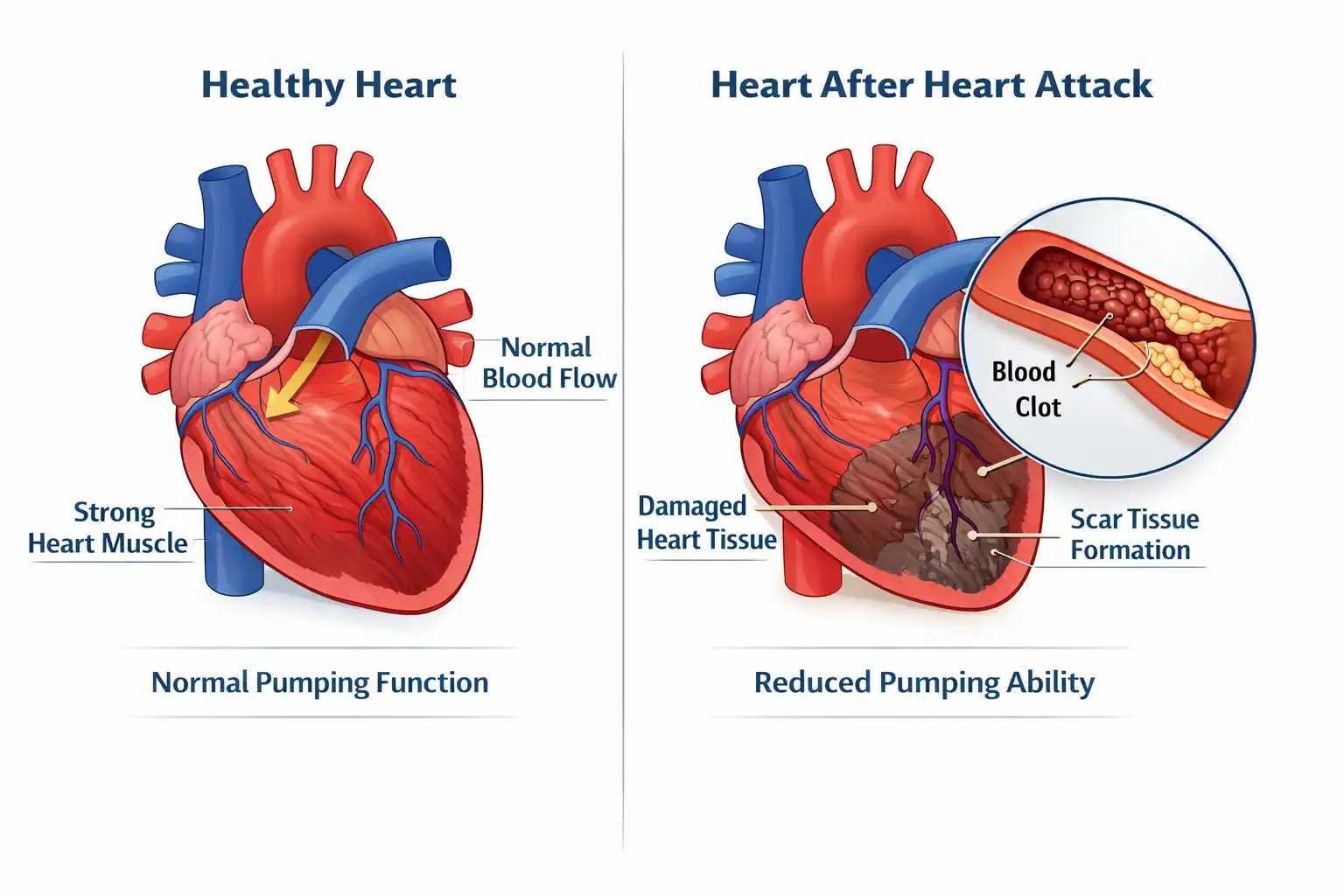
A heart attack occurs when blood flow to part of your heart muscle is blocked-usually by a blood clot. Without oxygen-rich blood, that section of heart muscle begins to die. Even after blood flow is restored, the damage leaves lasting effects on your heart's ability to pump effectively.
Here's the problem: heart muscle has very limited ability to regenerate on its own. Instead, scar tissue forms-and scar tissue doesn't contract like healthy heart muscle.
This can lead to reduced pumping efficiency (lower ejection fraction), fatigue and weakness from decreased blood flow, shortness of breath with exertion, irregular heartbeats, and increased risk of heart failure over time.
Medications and lifestyle changes help many people manage these symptoms. But many patients still struggle with reduced heart function that impacts their daily life-climbing stairs, playing with grandchildren, doing the activities they once enjoyed.
If you've tried standard treatments without regaining the function you need, stem cell therapy may be worth understanding.
What Stem Cell Therapy Is
Stem cell therapy is a treatment that aims to support your heart's natural repair processes. The cells used are adult mesenchymal stem cells derived from carefully screened placental tissue. These are not embryonic stem cells.
The old thinking about stem cells was simple: inject new cells, they become new tissue. New heart muscle. Like replacing worn parts.
The current understanding is different-and actually more promising.
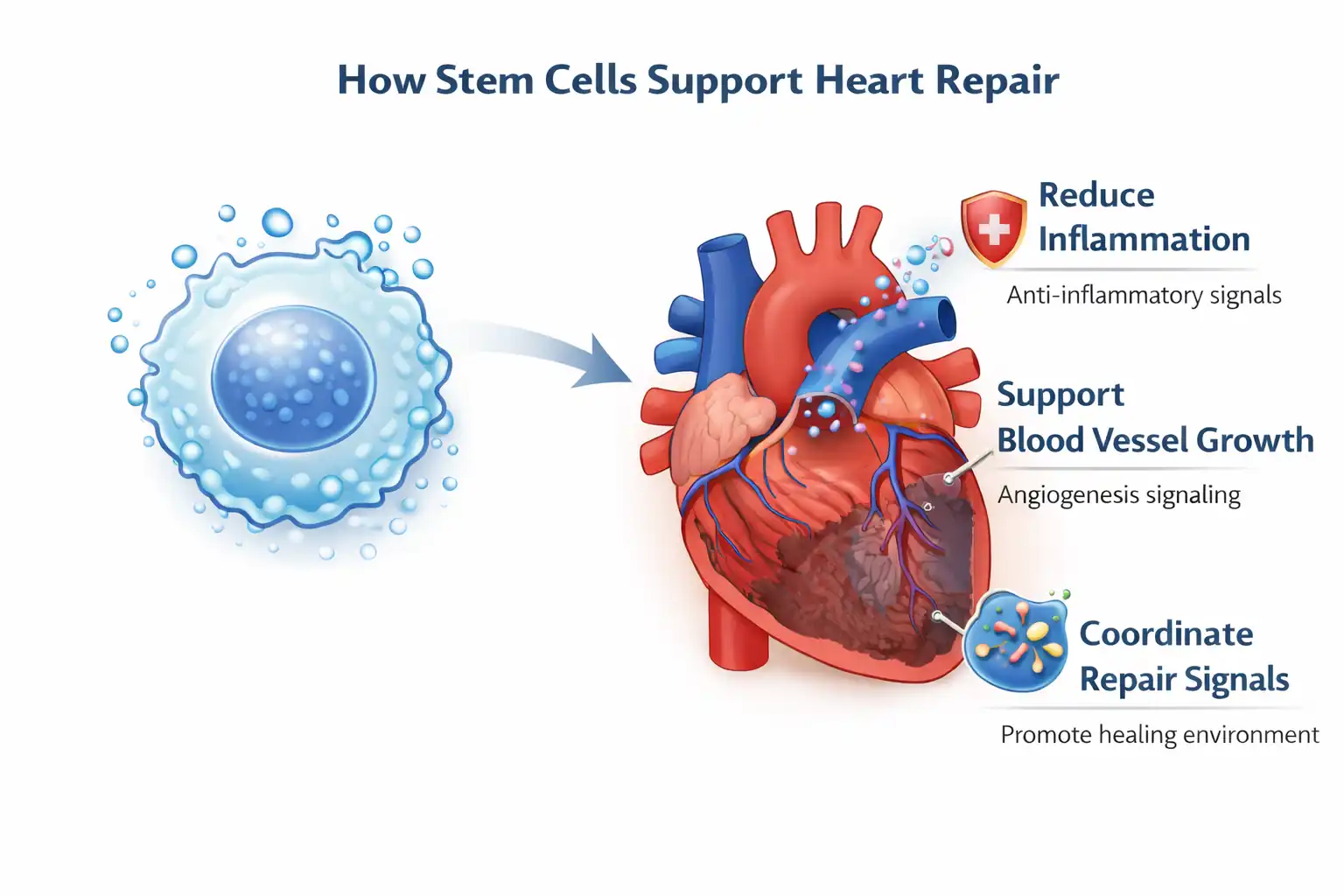
While stem cells may develop into new tissue cells to a limited degree, that's not their main value. What makes them therapeutically useful is their ability to coordinate and support your body's own healing. Your body already has repair mechanisms. The problem after a heart attack is that the damage is severe and the heart's natural regeneration capacity is limited.
What stem cells actually do:
- Release anti-inflammatory signals that may help reduce ongoing damage to heart tissue
- Recruit and activate your body's own repair cells at the injury site
- May support the growth of new blood vessels to improve blood flow
- Release growth factors that support heart cell survival and function
- Help reduce harmful oxidative stress that causes additional damage
- Aim to create conditions for healthier repair rather than excessive scar formation
Think of stem cells less like replacement parts and more like project managers. They assess the damage, calm the inflammation, call in resources, and help coordinate the reconstruction. They don't need to become new heart muscle to be effective-if they can shift the tissue environment from "damage mode" to "repair mode," your body's existing mechanisms may do better healing.
This is also why some patients notice improvement in the weeks following treatment. Early benefits often reflect reduced inflammation and improved tissue environment. Longer-term improvements may reflect actual tissue repair and improved heart function.
Who This Is (and Isn't) For
May be appropriate if you:
- Have experienced a heart attack and continue to have reduced heart function
- Have tried standard treatments (medications, cardiac rehab) without sufficient improvement
- Want to explore options to support heart healing
- Are in stable condition and cleared by your cardiologist
- Have realistic expectations about timeline and outcomes
Probably not appropriate if you:
- Are in the acute phase of a heart attack (this is for recovery support, not emergency treatment)
- Have unstable cardiac conditions that need to be addressed first
- Haven't yet tried standard cardiac rehabilitation
- Are looking for a guaranteed cure
How Stem Cells May Help With Heart Attack Damage
Reducing Heart Inflammation
The problem: After a heart attack, inflammation can cause additional damage to your heart. While some inflammation is part of the healing process, excessive or prolonged inflammation damages more heart tissue and contributes to scar formation.
What you experience: Ongoing fatigue, continued shortness of breath, slow recovery despite following your treatment plan.
How stem cells may help: Stem cells release anti-inflammatory molecules such as IL-10 and TGF-β that help calm down immune cells contributing to ongoing inflammation. By reducing this inflammatory burden, stem cells may protect your heart from further damage and create conditions where healing can occur more effectively.
Supporting Blood Vessel Growth
The problem: Heart attacks damage not just muscle but also the blood vessels that supply it. Poor blood flow to damaged areas limits the nutrients and oxygen available for healing and function.
What you experience: Reduced exercise tolerance, fatigue with activities that require your heart to work harder, slow improvement in stamina.
How stem cells may help: Stem cells release factors like VEGF (vascular endothelial growth factor) that may support the growth of new blood vessels-a process called angiogenesis. Better blood supply means better oxygen and nutrient delivery to healing tissue, potentially improving heart function over time.
Reducing Oxidative Stress
The problem: Heart attacks create oxidative stress-an imbalance that causes additional cellular damage. This oxidative damage continues to harm heart tissue even after the initial event, contributing to ongoing dysfunction.
What you experience: The cumulative effects of oxidative damage contribute to reduced heart function and slower recovery.
How stem cells may help: Stem cells may help reduce oxidative damage by promoting your body's natural antioxidant defenses. Less oxidative stress means less additional damage to your recovering heart, giving your body a better chance to heal.
Improving Overall Heart Function
The problem: The combined effects of muscle damage, scar tissue, inflammation, and reduced blood supply all contribute to decreased pumping efficiency. Your heart can't move blood as effectively as it once did.
What you experience: Lower ejection fraction on tests, fatigue, shortness of breath, reduced ability to do physical activities, swelling in legs or ankles.
How stem cells may help: By addressing multiple aspects of heart damage simultaneously-reducing inflammation, supporting blood vessel growth, fighting oxidative stress, and coordinating repair signals-stem cells aim to create conditions where your heart function may improve. Stem cells also release tiny packages called exosomes that carry healing factors directly to damaged areas, providing targeted support where it's needed most.
What the Procedure Is Like
Stem cell therapy for heart attack recovery is performed as an outpatient procedure. The treatment is administered intravenously, allowing the stem cells to travel through your bloodstream to your heart.
Here's what to expect:
1. Consultation and evaluation The medical team reviews your cardiac history, imaging, current medications, and overall health to determine if stem cell therapy is appropriate for your situation. You'll need clearance from your cardiologist.
2. Stem cell preparation We use mesenchymal stem cells derived from carefully screened placental tissue. These cells are processed and prepared for administration.
3. Treatment administration Stem cells are administered intravenously in a controlled clinical setting. The procedure typically takes 1-2 hours. You'll be monitored throughout.
4. Post-treatment Brief monitoring period, then home with specific instructions for activity and follow-up care. Most patients can return to normal activities within a day or two.
How is this different from standard heart medications?
Heart medications help manage symptoms and prevent further damage-they're important and you should continue them as prescribed. But they don't actively support tissue repair. Stem cell therapy aims to support your heart's healing processes, potentially improving function rather than just managing the status quo.
Recovery Timeline: What to Expect
Stem cell therapy for heart recovery works gradually. Your heart needs time to respond. Be patient.
First 24-48 hours Rest and take it easy. Some patients feel fatigued after treatment. This is normal.
Weeks 1-4 Continue your normal cardiac medications and follow your cardiologist's recommendations. Some patients notice early improvements in energy levels; others don't yet. Both are normal. The stem cells are beginning their work.
Months 1-3 Anti-inflammatory effects may become noticeable. Many patients report improved energy, reduced shortness of breath, and better exercise tolerance during this window. Continue cardiac rehabilitation if recommended.
Months 3-6 This is often when more significant improvements occur. Heart function measurements may show improvement. Stamina and daily function may continue to get better.
Months 6-12 Peak benefits typically appear for those who respond well. Improvements tend to stabilize at a new baseline.
Important: Individual responses vary considerably. Some patients see noticeable improvement; others experience more modest changes. Heart damage severity, time since heart attack, overall health, and other factors all influence outcomes. This therapy works alongside-not instead of-your standard cardiac care.
How This Compares to Other Options
The key difference: Medications and lifestyle changes are essential-they manage your condition and prevent further damage. Cardiac rehab improves your fitness and quality of life. Surgery addresses severe structural problems. Stem cell therapy aims to support actual tissue repair and improved heart function-a different approach that works alongside your standard care, not instead of it.
Bottom Line: Is This Worth Considering?
Stem cell therapy for heart attack recovery isn't a guaranteed fix. It's one option among several-and it's not right for everyone.
It may be worth considering if:
- You've had a heart attack and continue to have reduced heart function despite standard treatments
- You want to explore options that may support actual heart repair
- You're in stable condition and cleared by your cardiologist
- You're willing to give your body time to respond (weeks to months)
- You have realistic expectations about outcomes
The proposed mechanisms are biologically plausible. Research shows promise. The safety profile appears favorable when properly administered. Many patients report meaningful improvement in energy, stamina, and quality of life.
But "many" isn't "all." Results vary based on the extent of damage, time since heart attack, your overall health, and factors we don't fully understand yet. This is an evolving field.
If you're interested, a consultation can help determine whether this approach makes sense for your specific situation-and set realistic expectations about what it can and can't do. This therapy works alongside your standard cardiac care, not instead of it.
Statements not evaluated by FDA or COFEPRIS.
Treatment
- Medical consultation
- 300 million Stem Cell IV + 10billion exosomes
- EKG, Echocardiogram, chest x-ray then analysis with cardiologist and internist
- NAD + Glutathione + High Dose Vitamin C IV + others as need
- Full Blood Panel
- Recommended supplement to take.
- Recommendation on things to do to enhance wellness.
