Orthopedic
Stem Cell Treatment
Stem Cell Therapy for Thumb Pain: What You Need to Know
Why Thumb Pain Is Such a Big Deal
Your thumb accounts for up to 40% of your hand's function. That single digit is what allows you to grip, pinch, and manipulate objects with precision. When it hurts, everything gets harder-opening jars, turning keys, gripping a steering wheel, texting, writing, buttoning a shirt.
The thumb's basal joint (where it meets your wrist) is particularly vulnerable. It withstands up to 12 times the force you actually apply when pinching. A 10-pound pinch puts 120 pounds of stress on that joint. Over time, this takes a toll.
If you've tried splints, cortisone shots, or physical therapy without lasting relief-and you're not ready for surgery-stem cell therapy may be worth understanding.
What Stem Cell Therapy Is (Plain English)
Stem cell therapy is an injection-based treatment that aims to support your body's natural repair processes. The cells used are adult mesenchymal stem cells-sourced from your own tissue (bone marrow or fat) or from carefully screened donor tissue. These are not embryonic stem cells.
The old thinking about stem cells was simple: inject new cells, they become new tissue. Cartilage. Tendon. Ligament. Like replacing worn parts.
The current understanding is different-and actually more promising.
While stem cells may develop into new tissue cells to a limited degree, that's not their main value. What makes them therapeutically useful is their ability to coordinate and support your body's own healing. Your body already has repair mechanisms. The problem in chronic conditions is that something is blocking them-persistent inflammation, poor blood supply, accumulated damage that overwhelms the system.
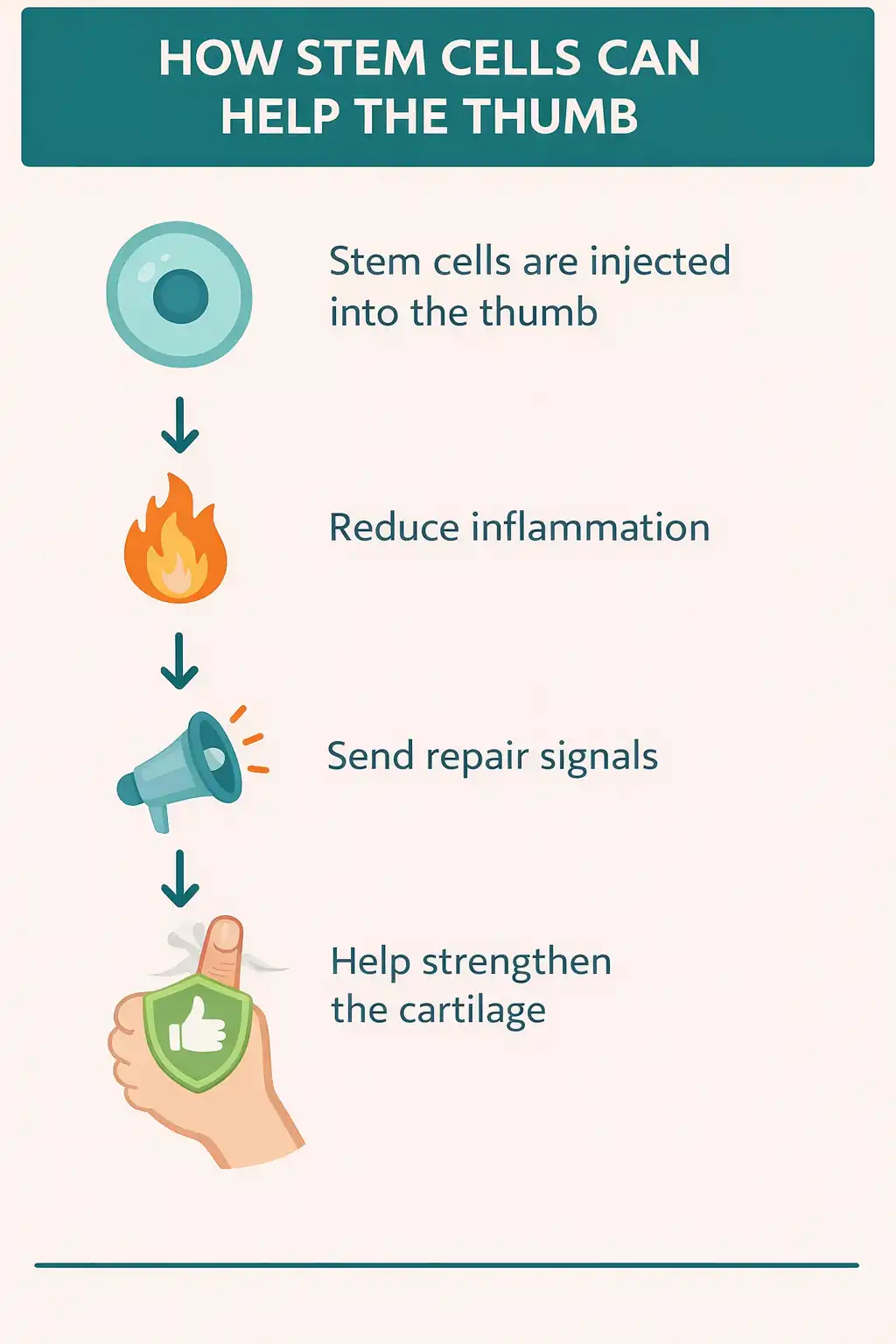
What stem cells actually do:
- Release anti-inflammatory signals that may help break chronic pain cycles
- Recruit and activate your body's own repair cells at the injury site
- May improve blood flow and nutrient delivery to damaged tissue
- Release growth factors that support tissue rebuilding
- Aim to create conditions for healthier repair rather than scar formation
Think of stem cells less like replacement parts and more like project managers. They assess the damage, calm the inflammation, call in resources, and help coordinate the reconstruction. They don't need to become new cartilage to be effective-if they can shift the tissue environment from "breakdown mode" to "repair mode," your body's existing mechanisms may do the rebuilding.
This is also why some patients notice improvement faster than expected. Early benefits often reflect reduced inflammation. Longer-term improvements may reflect actual tissue repair.
Who This Is (and Isn't) For
May be appropriate if you:
- Have thumb pain that hasn't improved with conservative treatments
- Want to explore options before considering surgery
- Need to maintain hand function for work or daily life
- Have realistic expectations about timeline and outcomes
Probably not appropriate if you:
- Have an acute injury that might heal on its own
- Haven't tried basic treatments yet (rest, splinting, therapy)
- Have severe end-stage arthritis with bone-on-bone damage
- Want an instant fix
How It May Help Common Thumb Conditions
Arthritis and Cartilage Damage
The problem: The most common form of thumb arthritis affects the basal joint-where your thumb meets your wrist. Healthy cartilage provides a smooth, cushioned surface that lets bones glide effortlessly. When arthritis develops, that cartilage wears down. Bone starts grinding on bone. The body responds with inflammation, which causes more damage, which triggers more inflammation-a vicious cycle that conventional treatments often struggle to break.
Cartilage is notoriously bad at healing itself. It has limited blood supply and few resident repair cells. This is why arthritis tends to progress rather than improve.
What you feel: Pain at the thumb base when gripping or pinching. Swelling and tenderness. Morning stiffness that eases as you move. Weakness when opening jars or turning keys. A grinding sensation during movement.
How stem cells may help: When stem cells are introduced into an arthritic joint, they may release anti-inflammatory signals that help break the damage cycle. They may also release growth factors that support existing cartilage cells and encourage matrix production. By improving the joint's internal environment-reducing inflammation, recruiting native repair cells, potentially improving nutrient delivery-stem cells aim to shift the joint from breakdown mode to maintenance mode.
The goal isn't necessarily to regrow lost cartilage (though some improvement may occur). It's to calm the destructive cycle, support what cartilage remains, and potentially slow further degeneration.
Ligament Injuries (Skier's Thumb / Gamekeeper's Thumb)
The problem: Your thumb has several critical ligaments, but the ulnar collateral ligament (UCL) gets injured most often. This typically happens when the thumb gets bent forcefully backward or sideways-common in falls (hence "skier's thumb") or repetitive stress.
Ligaments are tough, fibrous bands connecting bone to bone. When they tear, the joint loses stability. The thumb can still move, but it can't provide reliable grip strength. And ligaments heal slowly. The scar tissue that forms is typically weaker and less elastic than native ligament-which is why these injuries can lead to long-term instability even after "healing."
What you feel: Pain on the inner side of your thumb. Instability when gripping-things slip from your hand. Swelling and bruising. Difficulty with pinching motions. Weakness that doesn't improve with rest.
How stem cells may help: Stem cells may support ligament repair by releasing factors that promote fibroblast activity (fibroblasts are the cells that build ligament tissue) and support collagen production-the protein that gives ligaments their strength. They may also help modulate excessive scar tissue formation, creating conditions for more organized, functional repair.
The goal is to support a healing process that results in stronger, more stable tissue than would occur without intervention.
Tendon Problems (De Quervain's / Trigger Thumb)
The problem: Tendons connect muscle to bone-they transmit force from your forearm muscles to move your thumb. Two conditions are most common:
De Quervain's tenosynovitis affects the tendons on the thumb side of your wrist. The tendon sheath becomes inflamed and swollen, creating friction with every movement.
Trigger thumb involves the flexor tendon that bends your thumb. Inflammation causes the tendon to catch on a structure called the A1 pulley, creating a clicking, catching, or locking sensation.
Like ligaments, tendons heal slowly and imperfectly. Chronic tendon problems often involve both active inflammation and accumulated micro-damage that never fully repairs.
What you feel: Pain along the thumb side of your wrist. Clicking or catching when bending or straightening. Swelling near the base of the thumb. Pain that worsens with repetitive activities. Difficulty moving the thumb smoothly.
How stem cells may help: Stem cells may help by releasing anti-inflammatory signals that calm the irritated tissue. They may also release factors that encourage tendon cell activity and support collagen production. Improved blood supply to the area may enhance nutrient delivery. By shifting the tissue environment from chronic inflammation to active repair, stem cells aim to address underlying damage-not just symptoms.
Muscle Injuries
The problem: The muscles that power your thumb live mostly in your forearm, but the thenar muscles-that fleshy pad at the base of your thumb-provide crucial fine motor control. These muscles can be strained from overuse (repetitive gripping, typing, tool use) or acute injury.
Muscle has better healing capacity than cartilage, ligament, or tendon. But significant injuries can still result in persistent weakness and scar tissue that limits function.
What you feel: Pain with thumb movement. Weakness in grip strength. Difficulty with fine motor tasks. Muscle spasms or cramping. Fatigue during activities that used to be easy.
How stem cells may help: Stem cells may support muscle repair by releasing factors that promote muscle precursor cell activity and support the production of contractile proteins. Anti-inflammatory signaling may help reduce fibrosis (scar tissue formation within muscle). By improving the healing environment, stem cells aim to support more complete recovery with better functional outcomes.
What the Procedure Is Like
Stem cell therapy for thumb conditions is an outpatient procedure. No general anesthesia. No hospital stay. Most people return to normal activities within a day or two.
Here's what to expect:
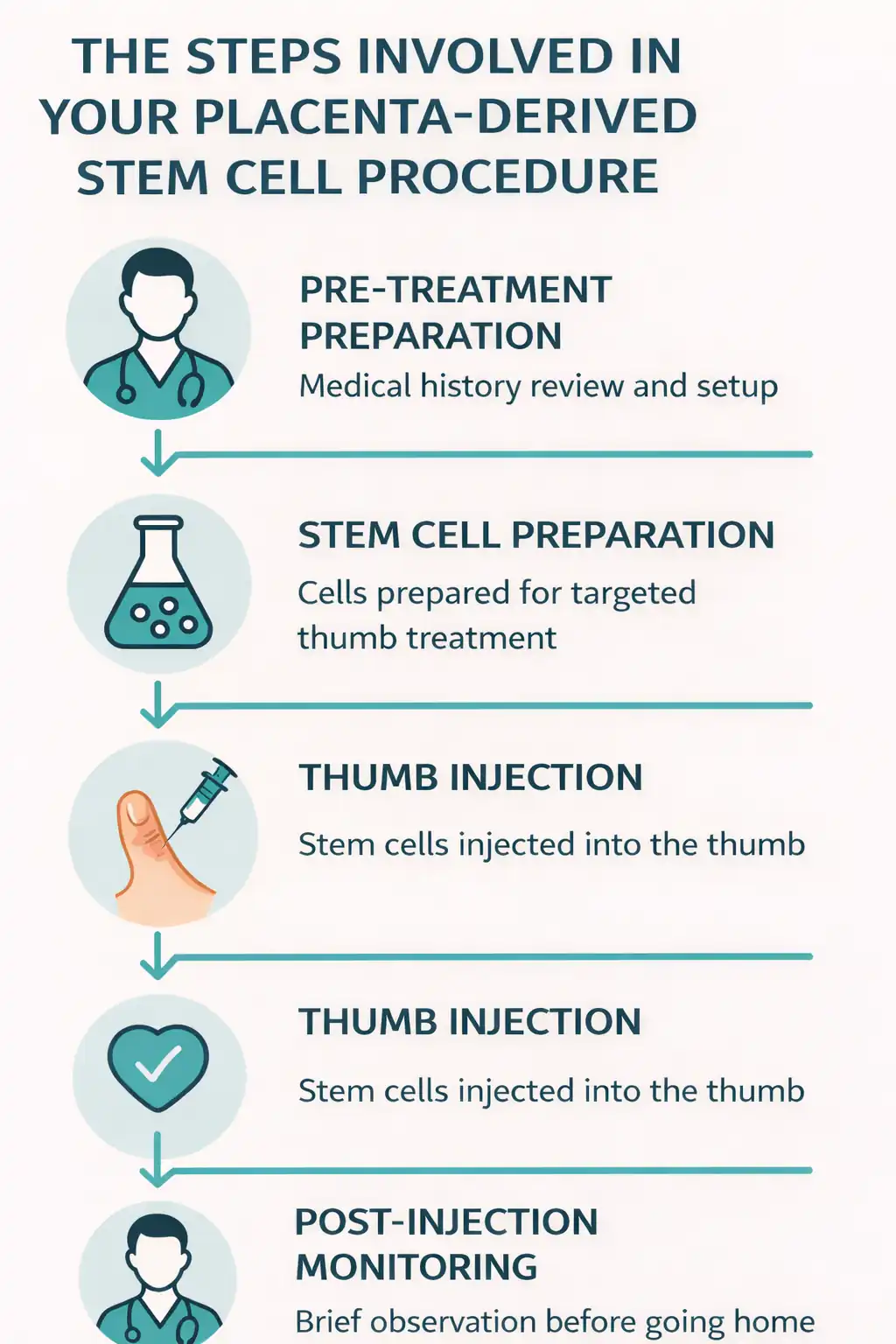
1. Consultation and evaluation The medical team reviews your condition, imaging, and treatment history to determine if stem cell therapy is appropriate for your situation.
2. Stem cell preparation We use mesenchymal stem cells derived from carefully screened placental tissue. These cells are processed and concentrated for injection.
3. Injection procedure Using ultrasound guidance for precision, stem cells are injected directly into the affected thumb joint, ligament, or tendon. The procedure typically takes 30-60 minutes.
4. Post-treatment Brief monitoring period, then home with specific instructions for activity modification and follow-up care.
The injection involves some discomfort-similar to any joint injection. Local anesthesia is used to minimize pain. Post-procedure soreness typically resolves within a few days.
How is this different from cortisone?
Cortisone reduces inflammation temporarily but doesn't support tissue repair. And repeated cortisone injections may actually weaken cartilage and tendons over time. Stem cell therapy aims to support the body's repair processes-not just suppress symptoms.
Recovery Timeline: What to Expect
Stem cell therapy isn't like taking a pill. The cells need time to do their work. This is a gradual process-be patient.
First 24-48 hours Some swelling and soreness at the injection site is normal and typically resolves quickly. Rest the thumb and avoid strenuous gripping.
Weeks 1-2 Gradual return to light activities. Some patients notice early improvement; others don't yet. Both are normal. The stem cells are establishing themselves and beginning their work.
Weeks 2-6 Anti-inflammatory effects become more noticeable. Many patients report reduced pain and improved function during this window. Gentle range-of-motion exercises typically begin.
Months 2-4 This is often when deeper tissue changes occur. Many patients experience their most significant improvements during this period. Strength and function may continue to improve.
Months 4-6 Peak benefits typically appear for those who respond well. Improvements tend to plateau-but at a higher baseline than before treatment.
Important: Individual responses vary considerably. Some conditions respond faster than others. Some patients see rapid improvement; others experience gradual change over months. Unlike cortisone (which works in days but wears off), stem cell therapy works over months and aims for more lasting improvement.
How This Compares to Other Options
The key difference: Cortisone manages symptoms temporarily-it reduces inflammation but doesn't repair tissue, and repeated use may actually weaken structures over time. Physical therapy builds strength but can't fix structural damage. Surgery can address severe problems but requires significant recovery time and carries risks.
Stem cell therapy occupies a middle ground. It's more active than conservative care, less invasive than surgery, and aims to support actual tissue repair rather than just mask symptoms.
Bottom Line: Is This Worth Considering?
Stem cell therapy isn't a guaranteed fix. It's one option among several-and it's not right for everyone.
It may be worth considering if:
- You've struggled with conventional treatments without lasting relief
- You want to avoid or delay surgery
- You need to maintain hand function for work or daily activities
- You're willing to give your body time to respond (weeks to months, not days)
- You have realistic expectations about outcomes
The proposed mechanisms are biologically plausible. The safety profile appears favorable. Many patients report meaningful improvement in function and quality of life.
But "many" isn't "all." Results vary based on the condition, its severity, your overall health, and factors we don't fully understand yet. This is an evolving field.
If you're interested, a consultation can help determine whether this approach makes sense for your specific situation-and set realistic expectations about what it can and can't do.
Individual results vary. No outcomes guaranteed. For educational purposes only-not medical advice. Consult a qualified provider to determine if appropriate for you. Statements not evaluated by FDA or COFEPRIS.
Treatment
- Medical consultation
- 25 million Mesenchymal StemCells + PRP applied via intra-articular injection.
- X-Ray
- Physiotherapyrecommendations
- Recommended supplement to take.
- Recommendation on things to do to enhance wellness.
